
Nursing Management of Children with Gastrointestinal Problems
Common Gastrointestinal Disorders in Children
Colostomy / Ostomy
Common Gastrointestinal Disorders in Children
Colostomy / Ostomy
Appendicitis
Celiac Disease
Crohn’s Disease
Hirschprung’s Disease
Intussusception
Colostomy / Ostomy
An ostomy is an opening in the intestine with the intestinal wall drawn to the abdomen. A stoma is created to allow passage of intestinal contents. An ostomy can be temporary or permanent, depending on the reason for the ostomy and how much of the intestine is being removed.
Indications
To correct an anatomical defect, relieve an obstruction, or permit treatment of an infection or injury to the intestinal tract. The most common reasons for an ostomy in infants and children are imperforate anus, necrotizing enterocolitis, HD, and inflammatory bowel disease.
Location
`An ILEOSTOMY is placed in the ileum portion of the small intestine
A COLOSTOMY is placed in the large intestine and may be ascending, transverse, or descending depending on were it is placed.
Nursing Considerations
nExplain the procedure in simple, age-appropriate terms, preparing the child and his parents for all aspects of the surgery
nCare of the Ostomy: Record the amount, character, color, and odor of the drainage, wash the stoma with soap and water, rinse, pat dry, Apply a protective ointment for irritation.
nA low residue diet maybe required, avoid gas producing foods
APPENDICITIS
Celiac Disease
Crohn’s Disease
Hirschprung’s Disease
Intussusception
Colostomy / Ostomy
An ostomy is an opening in the intestine with the intestinal wall drawn to the abdomen. A stoma is created to allow passage of intestinal contents. An ostomy can be temporary or permanent, depending on the reason for the ostomy and how much of the intestine is being removed.
Indications

To correct an anatomical defect, relieve an obstruction, or permit treatment of an infection or injury to the intestinal tract. The most common reasons for an ostomy in infants and children are imperforate anus, necrotizing enterocolitis, HD, and inflammatory bowel disease.
Location
`An ILEOSTOMY is placed in the ileum portion of the small intestine
A COLOSTOMY is placed in the large intestine and may be ascending, transverse, or descending depending on were it is placed.
Nursing Considerations
nExplain the procedure in simple, age-appropriate terms, preparing the child and his parents for all aspects of the surgery
nCare of the Ostomy: Record the amount, character, color, and odor of the drainage, wash the stoma with soap and water, rinse, pat dry, Apply a protective ointment for irritation.
nA low residue diet maybe required, avoid gas producing foods
APPENDICITIS

It is an inflammation and obstruction of the blind sac (Vermiform Appendix) at the end of the cecum. It is the most common major surgical disease in school age children and its peak incidence occurs in children between 10 and 12 years. Although the appendix has no known function, it does regularly fill and empty itself with food.
Cause
The Appendiceal Lumen becomes obstructed with fecal matter, calculi, tumors, or strictures from trauma or infection due to bacteria, viruses or parasites.
It could also lead to infection, thrombosis, necrosis, and perforation. If the Appendix ruptures or perforates, the infected contents spill into the abdominal cavity causing peritonitis.
Signs and Symptoms
Mid abdominal cramps and tenderness are diffuse eventually they localize in the RLQ at Mc burney’s point.
Nausea and Vomiting
Low grade fever
Lethargy
Irritability
Constipation and rarely diarrhea
Tests to determine
nBased on physical findings and characteristic clinical symptoms
nA moderately elevated WBC with increased numbers of immature cells supports the diagnosis
Nursing Considerations
Explain the procedure at a level of understanding
Tell the child or the parents what to expect when he awakens (IV line, NGT)
Position the Child pre-operatively in a semi fowlers or side lying position with knees bent to decrease pain
Administer IV Fluids to prevent dehydration and keep the patient on NPO status until surgery is performed
Never apply heat to the right lower abdomen, this may cause the appendix to rupture.
Postoperative Care must be done.
Celiac Disease
It is an inborn error in the metabolism characterized by poor absorption and intolerance of gluten ( a protein found in grains, such as wheat, rye, oats and barley ). The disease usually becomes apparent between ages 6 and 18 months, after gluten containing foods are introduced in the diet.
Causes
This relatively uncommon disorder probably results from environmental factors and a genetic predisposition.
The 1st Theory: The disease involves an abnormal immune response.
The 2nd Theory: It proposes that an intramucosal enzyme defect produces an inability to digest gluten.
Signs and Symptoms
nRecurrent attacks of Diarrhea
nSteatorrhea (fatty, foul smelling stools)
nAbdominal pain and distention
nVomiting
nAnorexia
nIrritability
nCoagulation difficulties from the malabsorption of fat soluble vitamins
nInspection reveals signs of generalized malnutrition and failure to thrive, such as potbelly or muscle wasting
Laboratory exams
nHistologic changes seen on small bowel biopsy specimens confirm the diagnosis
nA Glucose Tolerance Test shows poor glucose absorption
nSerum lab tests indicate decrease in levels of albumin, calcium, sodium, potassium, cholesterol and phospholipids.
nHemoglobin level, hematocrit, WBC counts, and platelet counts may also be decreased
nImmunologic Assay screen (immunoglobulin {Ig} A and IgG antibodies) is positive for celiac disease.
nStool specimens reveal a high fat content.
Nursing Consideration
The main focus of Celiac Disease focus primarily on educating the parents about caring for the children at home with emphasis on the ff:
Eliminate gluten in the Diet
Provide a diet that includes corn and rice products, soy and potato flour, and fresh fruits and vegetables, for the infant, give breast milk or soy based formula.
Replace vitamins and calories, give small, frequent meals
Monitor for steatorrhea, its disappearance is a good indicator that the childs ability to absorb nutrients is improving
Crohn’s Disease
It is a chronic inflammation and ulceration of the GI tract anywhere from the mouth to the anus usually involving the terminal ileum. The disease extends through all layers of the intestinal wall and may involve regional lymph nodes and the mesentery
Causes
Exact cause is unknown
Allergies and other immune disorders
Infection (although no infecting organism has been identified)
Genetic factors plays a role
An inflammatory response causes mucosal ulcers to grow in size and depth in the mucosal wall of the GI tract. Fibrosis and stiffening of the mucosal wall can occur . Fistulas can develop between bowel loops or adjoining organs
Signs and symptoms
Acute symptoms include steady, colicky pain in the RLQ (cramping), diarrhea and flatulence, fever and bloody stool.
Chronic symptoms includes diarrhea (four to six stools per day), pain in the RLQ, excess fat in stool, weight loss, weakness and fatigue, cramping, and abdominal distention.
Treatment
Administration of corticosteroids, aminosalicylates, anti-infectives, and immunosuppressive agents.
Nutritional Support
TPN may be administered
Surgical Treatment : bowel resection for obstructions or fistulas or a total colectomy with ileostomy if the bowel perforates. (surgery doesn’t cure Crohn’s disease but relieves symptoms temporarily until the next exacerbation).
Nursing Consideration
Administer analgesics and antispasmodics to decrease abdominal pain and corticosteroids to decrease bowel inflammation as ordered.
Withhold food and fluids, using parenteral nutrition in place of feeding to rest the bowel.
Teach proper nutritional support to the child and his parents incldg. The need of small frequent meals that are high protein, high calorie and low fiber
Promote stress reduction through relaxation and distraction.
Hirschprung’s Disease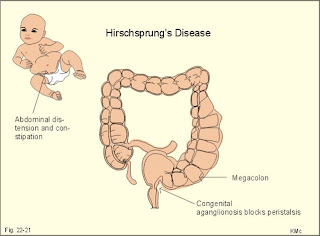
It is the absence of parasympathetic ganglionic cells in a segment of the colon, usually at the distal end of the large intestine. The lack of nerve innervation causes an absence of, or alteration in, peristalsis in the affected part of the colon.
Causes
It is believed to be a result of a congenital usually familial defect. The disease may coexist with other congenital anomalies, particularly Down Syndrome and anomalies of the urinary tract.
How it happens?
What test tell you?
Rectal biopsy provides a definitive diagnosis by showing the absence of ganglion cells
nSuction aspiration, using a small tube inserted into the rectum, also determines the absence of ganglion cells
Full thickness surgical biopsy uder GA
Rectal manometry reveals failure of the internal anal sphincter to relax and contract
Abdominal X-rays show distention of the colon
Complications
nSevere diarrhea
nBowel perforation
nSepsis
nIncontinence
nStricture formation
nEnterocolitis
nHypovolemic Shock
Treatment
SURGERY is the treatment of choice in these children and should performed as soon as the child’s fluid and electrolyte imbalances are stabilized.
Nursing Considerations
PREOPERATIVE CARE
nAdminister IV Fluids to maintain fluid and electrolyte balance and prevent dehydration and shock
nMaintain on NPO status and insert an NGT for gastric decompression.
nAdminister isotonic enemas (PNSS) to evacuate the bowels **Don’t administer tap water due to the risk of water intoxication
nAdminister antibiotics as ordered
POSTOPERATIVE CARE
After a colostomy / ileostomy, follow these steps:
nMonitor I & O ; an ileostomy is especially likely to cause excessive electrolyte loss.
nKeep the area around the stoma clean and dry
nMonitor for return of bowel sounds to begin diet
nNo rectal dilatations, rectal thermometer and suppositories
Intussusception
nIs a telescoping or invagination of a bowel segment into itself. It occurs at about age 6 months but it can occur in children up to 3 years old
nIt is 3x more likely to occur in Males than in females.
On inspection and palpation may reveal a distended and tender abdomen with a palpable “sausage shaped abdominal mass” Other clinical signs include:
nFever
nIncreased pulse
nShallow respirations
nDecreased blood Pressure
nAbdominal X-rays show a soft tissue mass and signs of complete or partial obstruction.
nBarium Enema confirms colonic intussusception when its shows the characteristic coiled spring sign
nA WBC as high than 15 indicates obstruction
nA WBC higher than 15 indicates strangulation
nA WBC higher than 20 indicates bowel infarction
Treatment
nNGT is inserted to decompress the intestine and minimize vomiting.
nSurgery is indicated when hydrostatic reduction fails, intussusception recurs or signs of shock or peritonitis are present.
nIf manual reduction fails, or if the bowel segment is gangrenous or strangulated, resection is performed
Nursing Considerations
nPrepare for Enema insertion (barium or water soluble contrast medium) to confirm the diagnosis and reduce the invagination by hydrostatic pressure
nMonitor v/s ; a change in temperature may indicate sepsis
nMonitor I & O to prevent dehydration and administer IV fluids as ordered
nMonitor NGT lossess and replace volume lost cc/cc
nAdminister pain medications as ordered.
nMonitor the incision sites for signs of infection and such as inflammation, drainage and suture separation

Quick QUIZ???
A 12 year old boy is admitted to the pediatric unit with complaints of RLQ abdominal pain and vomiting. When the nurse checks on the child 2 hours later, he states that the pain has stopped. The nurse should suspect that:
nHe had indigestion, which has been relieved
nHe’s afraid of going to surgery
nHis appendix has ruptured
nHe has irritable bowel syndrome
ANSWER
nC - Abdominal pain in the RLQ and vomiting are symptoms of appendicitis. When the appendix ruptures a sudden relief of pain occurs, after which the pain resumes more severely.
An 18 month old child is admitted to the pediatric unit with intussusception. As the nurse is preparing the child for a barium contrast reduction, he passess a soft brown stool. What should the Nurse do?
nNotify the doctor in order to cancel the procedure
nPrepare the child for emergency surgery
nTake v/s and monitor for abdominal sounds
nAdminister an enema to clear the rectal area for testing
ANSWER
A – Passing a normal looking brown stool indicates that the child no longer has an invaginated section of bowel.
The Nurse is completing a discharge teaching for a child and her parents regarding her diet to treat celiac disease. Which meal selection would be appropriate for this child?
nA bologna sandwich on whole wheat bread, a chocolate chip cookie, and a glass of milk
nA vegetable pizza, an apple, and a diet cola
nA corn tortilla with hamburger and cooked vegetables, and a glass of fruit juice.
nA hotdog on a roll, celery, and carrot sticks and a chocolate milk shake
ANSWER
C - Celiac Disease is intolerance to wheat, barley, rye and oats. Some of this children also have lactose intolerance especially when they have an acute episode of the attack
KAWASAKI DISEASE
What is KAWASAKI DISEASE?
§Kawasaki Disease is an illness that involves the skin, mouth, and lymph nodes, and typically affects children who are under the age of 5. The cause of Kawasaki Disease is unknown, but if the symptoms are recognized early, kids with the disease can fully recover within a few days. If it goes untreated, it can lead to serious complications that can involve the heart.
§Kawasaki disease occurs in 19 out of every 100,000 kids in the Philippines. It is most common among children of Japanese and Korean descent, but the illness can affect all ethnic groups.
§Kawasaki disease is an uncommon disease affecting mainly preschool children, although older children can also get it. The cause is currently not known but research is being done to try and find out. It is probably a severe response to an infection, although we do not yet know which infection. It results in inflammation affecting many different blood vessels all over the body.
§The symptoms of Kawasaki Disease typically appear in phases.
§The first phase, which can last for up to 2 weeks, usually involves a persistent fever that is higher than 104 degrees Fahrenheit (39 degrees Celsius), and lasts for at least 5 days. The other symptoms that typically develop include:
§severe redness in the eyes
§a rash on the child's stomach, chest, and genitals
§red, dry, cracked lips
§swollen tongue with a white coating and big red bumps
§sore, irritated throat
§swollen palms of the hands and soles of the feet with a purple-red color
§swollen lymph nodes
Complications of Kawasaki Disease
§Doctors can manage the symptoms of Kawasaki disease if they catch it early. The symptoms typically disappear within just two days of when treatment begins. Usually, if Kawasaki disease is treated within 10 days of when the first symptoms begin, no heart problems develop.
§But if the illness goes untreated (time period can vary, but likely for 10-14 days and sooner in young infants), it can lead to more serious complications that involve the child's heart. Kawasaki disease can lead to vasculitis, which is an inflammation of the blood vessels. This can be particularly dangerous because it can affect the coronary arteries, which supply blood to the heart.
§In addition to the coronary arteries, the heart muscle, lining, valves, or the outer membrane that surrounds the heart can become inflamed. Arrhythmias (changes in the normal pattern of the heartbeat) or abnormal functioning of some heart valves can also occur.
Diagnosing Kawasaki Disease
§There is no one test to detect Kawasaki disease, so a doctor typically diagnoses it by evaluating the child's symptoms and ruling out other conditions.
§Typically, a child who is diagnosed with this illness will have a fever lasting 5 or more days and at least 4 of the following symptoms:
§if Kawasaki disease is suspected, a doctor may order tests to monitor the child's heart function, which can include an echocardiogram, and other tests of heart function. A doctor may also take blood and urine samples to rule out other conditions, such as scarlet fever, measles, Rocky Mountain Spotted Fever, Stevens-Johnson syndrome, juvenile rheumatoid arthritis, and an allergic drug reaction.
Treating KawasakiDisease
§Treatment should begin as soon as possible, ideally within 10 days of when the fever first begins. Usually, a child is treated with intravenous doses of gamma globulin (purified antibodies), an ingredient of blood that helps the child's body fight off infection. The child may also be given a high-dose of aspirin to reduce the risk of heart problems.
Gamma Globulin
Hyperalimentation / Total Parenteral Nutrition
TOTAL PARENTAL NUTRITION
Hyperalimentation
•Infusion of hypertonic solutions of dextrose, nitrogen and additives ( vitamins, minerals, electrolytes, essential trace elements) directly into the bloodstream through and indwelling venous catheter in order to restore/maintain normal body composition and nutrition in individuals who are unable to meet their needs via the gastrointestinal (GI) tract.
•Usually administered via an established central venous line or a right atrial catheter.
•Process of nourishing the body thru parental means.
•Hypertonic solutions need to be infused directly into a central vein with high blood flow.
•Less concentrated solutions may be given via peripheral vein.
Indications:
•When adequate oral enteral intake is impossible.
a. Chronic obstruction of the GI tract uncorrected or not correctable within 10 days in older children, 5 days in children below 5 years old.
- Gastric malignancies pending surgery
- Superior mesenteric artery syndrome
Intestinal atresia
- Malrotation of the bowels
Short bowel syndrome
Post irradiation effects on bowels pending surgery
Chemotherapy complications in bowels pending surgery
Massive catabolism
- Major burns
- Multiple major operations
- Multiple major trauma
•Congenital anomalies compatible with adequate oral intake later in life
- Omphalocoele
- Gastroschisis
- Diaphragmatic hernias
- Abdominal wound dehiscence7
•When oral enteral intake is not advisable
a. High output GI fistulas wherein oral or enteral feeding is inadequate
b. Extremely premature infants with surgical problems
NURSING RESPOSIBILITIES AND CARE OF PATIENT WITH TPN
•Prepare the patient and family emotionally and physically for the procedures.
- Explain procedure to patient and family to allay anxiety in developmentally appropriate terms.
- Allow the child and family to express concerns and feelings.
- Younger children may benefit from therapeutic play with a doll or puppet.
•Assist the physician during the catheter insertion.
- Prepare all materials / equipment needed.
•Ensure that physician’s orders are carried out.
- Check solution content with orders to ensure correct hyperalimentation solution additive before starting the infusion.
- Each TPN bottle must be labelled with patient’s name, room number, additives, IV number, date starting time and time to consume.
•Ensure that patient will receive adequate nutrition
- Monitor the volume/amount of solution hourly
- Inspect the peripheral TPN site for evidence of infiltration
Tell the child or the parents what to expect when he awakens (IV line, NGT)
Position the Child pre-operatively in a semi fowlers or side lying position with knees bent to decrease pain
Administer IV Fluids to prevent dehydration and keep the patient on NPO status until surgery is performed
Never apply heat to the right lower abdomen, this may cause the appendix to rupture.
Postoperative Care must be done.
Celiac Disease
It is an inborn error in the metabolism characterized by poor absorption and intolerance of gluten ( a protein found in grains, such as wheat, rye, oats and barley ). The disease usually becomes apparent between ages 6 and 18 months, after gluten containing foods are introduced in the diet.
Causes
This relatively uncommon disorder probably results from environmental factors and a genetic predisposition.
The 1st Theory: The disease involves an abnormal immune response.
The 2nd Theory: It proposes that an intramucosal enzyme defect produces an inability to digest gluten.
Signs and Symptoms
nRecurrent attacks of Diarrhea
nSteatorrhea (fatty, foul smelling stools)
nAbdominal pain and distention
nVomiting
nAnorexia
nIrritability
nCoagulation difficulties from the malabsorption of fat soluble vitamins
nInspection reveals signs of generalized malnutrition and failure to thrive, such as potbelly or muscle wasting
Laboratory exams
nHistologic changes seen on small bowel biopsy specimens confirm the diagnosis
nA Glucose Tolerance Test shows poor glucose absorption
nSerum lab tests indicate decrease in levels of albumin, calcium, sodium, potassium, cholesterol and phospholipids.
nHemoglobin level, hematocrit, WBC counts, and platelet counts may also be decreased
nImmunologic Assay screen (immunoglobulin {Ig} A and IgG antibodies) is positive for celiac disease.
nStool specimens reveal a high fat content.
Nursing Consideration
The main focus of Celiac Disease focus primarily on educating the parents about caring for the children at home with emphasis on the ff:
Eliminate gluten in the Diet
Provide a diet that includes corn and rice products, soy and potato flour, and fresh fruits and vegetables, for the infant, give breast milk or soy based formula.
Replace vitamins and calories, give small, frequent meals
Monitor for steatorrhea, its disappearance is a good indicator that the childs ability to absorb nutrients is improving
Crohn’s Disease
It is a chronic inflammation and ulceration of the GI tract anywhere from the mouth to the anus usually involving the terminal ileum. The disease extends through all layers of the intestinal wall and may involve regional lymph nodes and the mesentery
Causes
Exact cause is unknown
Allergies and other immune disorders
Infection (although no infecting organism has been identified)
Genetic factors plays a role
An inflammatory response causes mucosal ulcers to grow in size and depth in the mucosal wall of the GI tract. Fibrosis and stiffening of the mucosal wall can occur . Fistulas can develop between bowel loops or adjoining organs
Signs and symptoms
Acute symptoms include steady, colicky pain in the RLQ (cramping), diarrhea and flatulence, fever and bloody stool.
Chronic symptoms includes diarrhea (four to six stools per day), pain in the RLQ, excess fat in stool, weight loss, weakness and fatigue, cramping, and abdominal distention.
Treatment
Administration of corticosteroids, aminosalicylates, anti-infectives, and immunosuppressive agents.
Nutritional Support
TPN may be administered
Surgical Treatment : bowel resection for obstructions or fistulas or a total colectomy with ileostomy if the bowel perforates. (surgery doesn’t cure Crohn’s disease but relieves symptoms temporarily until the next exacerbation).
Nursing Consideration
Administer analgesics and antispasmodics to decrease abdominal pain and corticosteroids to decrease bowel inflammation as ordered.
Withhold food and fluids, using parenteral nutrition in place of feeding to rest the bowel.
Teach proper nutritional support to the child and his parents incldg. The need of small frequent meals that are high protein, high calorie and low fiber
Promote stress reduction through relaxation and distraction.
Hirschprung’s Disease
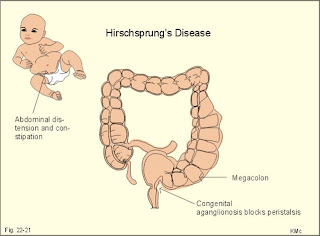
It is the absence of parasympathetic ganglionic cells in a segment of the colon, usually at the distal end of the large intestine. The lack of nerve innervation causes an absence of, or alteration in, peristalsis in the affected part of the colon.
Causes
It is believed to be a result of a congenital usually familial defect. The disease may coexist with other congenital anomalies, particularly Down Syndrome and anomalies of the urinary tract.
How it happens?

What test tell you?
Rectal biopsy provides a definitive diagnosis by showing the absence of ganglion cells
nSuction aspiration, using a small tube inserted into the rectum, also determines the absence of ganglion cells
Full thickness surgical biopsy uder GA
Rectal manometry reveals failure of the internal anal sphincter to relax and contract
Abdominal X-rays show distention of the colon
Complications
nSevere diarrhea
nBowel perforation
nSepsis
nIncontinence
nStricture formation
nEnterocolitis
nHypovolemic Shock
Treatment
SURGERY is the treatment of choice in these children and should performed as soon as the child’s fluid and electrolyte imbalances are stabilized.
Nursing Considerations
PREOPERATIVE CARE
nAdminister IV Fluids to maintain fluid and electrolyte balance and prevent dehydration and shock
nMaintain on NPO status and insert an NGT for gastric decompression.
nAdminister isotonic enemas (PNSS) to evacuate the bowels **Don’t administer tap water due to the risk of water intoxication
nAdminister antibiotics as ordered
POSTOPERATIVE CARE
After a colostomy / ileostomy, follow these steps:
nMonitor I & O ; an ileostomy is especially likely to cause excessive electrolyte loss.
nKeep the area around the stoma clean and dry
nMonitor for return of bowel sounds to begin diet
nNo rectal dilatations, rectal thermometer and suppositories
Intussusception

nIs a telescoping or invagination of a bowel segment into itself. It occurs at about age 6 months but it can occur in children up to 3 years old
nIt is 3x more likely to occur in Males than in females.
On inspection and palpation may reveal a distended and tender abdomen with a palpable “sausage shaped abdominal mass” Other clinical signs include:
nFever
nIncreased pulse
nShallow respirations
nDecreased blood Pressure

nAbdominal X-rays show a soft tissue mass and signs of complete or partial obstruction.
nBarium Enema confirms colonic intussusception when its shows the characteristic coiled spring sign
nA WBC as high than 15 indicates obstruction
nA WBC higher than 15 indicates strangulation
nA WBC higher than 20 indicates bowel infarction
Treatment
nNGT is inserted to decompress the intestine and minimize vomiting.
nSurgery is indicated when hydrostatic reduction fails, intussusception recurs or signs of shock or peritonitis are present.
nIf manual reduction fails, or if the bowel segment is gangrenous or strangulated, resection is performed
Nursing Considerations
nPrepare for Enema insertion (barium or water soluble contrast medium) to confirm the diagnosis and reduce the invagination by hydrostatic pressure
nMonitor v/s ; a change in temperature may indicate sepsis
nMonitor I & O to prevent dehydration and administer IV fluids as ordered
nMonitor NGT lossess and replace volume lost cc/cc
nAdminister pain medications as ordered.
nMonitor the incision sites for signs of infection and such as inflammation, drainage and suture separation

Quick QUIZ???
A 12 year old boy is admitted to the pediatric unit with complaints of RLQ abdominal pain and vomiting. When the nurse checks on the child 2 hours later, he states that the pain has stopped. The nurse should suspect that:
nHe had indigestion, which has been relieved
nHe’s afraid of going to surgery
nHis appendix has ruptured
nHe has irritable bowel syndrome
ANSWER
nC - Abdominal pain in the RLQ and vomiting are symptoms of appendicitis. When the appendix ruptures a sudden relief of pain occurs, after which the pain resumes more severely.
An 18 month old child is admitted to the pediatric unit with intussusception. As the nurse is preparing the child for a barium contrast reduction, he passess a soft brown stool. What should the Nurse do?
nNotify the doctor in order to cancel the procedure
nPrepare the child for emergency surgery
nTake v/s and monitor for abdominal sounds
nAdminister an enema to clear the rectal area for testing
ANSWER
A – Passing a normal looking brown stool indicates that the child no longer has an invaginated section of bowel.
The Nurse is completing a discharge teaching for a child and her parents regarding her diet to treat celiac disease. Which meal selection would be appropriate for this child?
nA bologna sandwich on whole wheat bread, a chocolate chip cookie, and a glass of milk
nA vegetable pizza, an apple, and a diet cola
nA corn tortilla with hamburger and cooked vegetables, and a glass of fruit juice.
nA hotdog on a roll, celery, and carrot sticks and a chocolate milk shake
ANSWER
C - Celiac Disease is intolerance to wheat, barley, rye and oats. Some of this children also have lactose intolerance especially when they have an acute episode of the attack
KAWASAKI DISEASE
What is KAWASAKI DISEASE?
§Kawasaki Disease is an illness that involves the skin, mouth, and lymph nodes, and typically affects children who are under the age of 5. The cause of Kawasaki Disease is unknown, but if the symptoms are recognized early, kids with the disease can fully recover within a few days. If it goes untreated, it can lead to serious complications that can involve the heart.
§Kawasaki disease occurs in 19 out of every 100,000 kids in the Philippines. It is most common among children of Japanese and Korean descent, but the illness can affect all ethnic groups.
§Kawasaki disease is an uncommon disease affecting mainly preschool children, although older children can also get it. The cause is currently not known but research is being done to try and find out. It is probably a severe response to an infection, although we do not yet know which infection. It results in inflammation affecting many different blood vessels all over the body.
§The symptoms of Kawasaki Disease typically appear in phases.
§The first phase, which can last for up to 2 weeks, usually involves a persistent fever that is higher than 104 degrees Fahrenheit (39 degrees Celsius), and lasts for at least 5 days. The other symptoms that typically develop include:
§severe redness in the eyes
§a rash on the child's stomach, chest, and genitals
§red, dry, cracked lips
§swollen tongue with a white coating and big red bumps
§sore, irritated throat
§swollen palms of the hands and soles of the feet with a purple-red color
§swollen lymph nodes
Complications of Kawasaki Disease
§Doctors can manage the symptoms of Kawasaki disease if they catch it early. The symptoms typically disappear within just two days of when treatment begins. Usually, if Kawasaki disease is treated within 10 days of when the first symptoms begin, no heart problems develop.
§But if the illness goes untreated (time period can vary, but likely for 10-14 days and sooner in young infants), it can lead to more serious complications that involve the child's heart. Kawasaki disease can lead to vasculitis, which is an inflammation of the blood vessels. This can be particularly dangerous because it can affect the coronary arteries, which supply blood to the heart.
§In addition to the coronary arteries, the heart muscle, lining, valves, or the outer membrane that surrounds the heart can become inflamed. Arrhythmias (changes in the normal pattern of the heartbeat) or abnormal functioning of some heart valves can also occur.
Diagnosing Kawasaki Disease
§There is no one test to detect Kawasaki disease, so a doctor typically diagnoses it by evaluating the child's symptoms and ruling out other conditions.
§Typically, a child who is diagnosed with this illness will have a fever lasting 5 or more days and at least 4 of the following symptoms:
§if Kawasaki disease is suspected, a doctor may order tests to monitor the child's heart function, which can include an echocardiogram, and other tests of heart function. A doctor may also take blood and urine samples to rule out other conditions, such as scarlet fever, measles, Rocky Mountain Spotted Fever, Stevens-Johnson syndrome, juvenile rheumatoid arthritis, and an allergic drug reaction.
Treating KawasakiDisease
§Treatment should begin as soon as possible, ideally within 10 days of when the fever first begins. Usually, a child is treated with intravenous doses of gamma globulin (purified antibodies), an ingredient of blood that helps the child's body fight off infection. The child may also be given a high-dose of aspirin to reduce the risk of heart problems.
Gamma Globulin
Hyperalimentation / Total Parenteral Nutrition
TOTAL PARENTAL NUTRITION
Hyperalimentation
•Infusion of hypertonic solutions of dextrose, nitrogen and additives ( vitamins, minerals, electrolytes, essential trace elements) directly into the bloodstream through and indwelling venous catheter in order to restore/maintain normal body composition and nutrition in individuals who are unable to meet their needs via the gastrointestinal (GI) tract.
•Usually administered via an established central venous line or a right atrial catheter.
•Process of nourishing the body thru parental means.
•Hypertonic solutions need to be infused directly into a central vein with high blood flow.
•Less concentrated solutions may be given via peripheral vein.
Indications:
•When adequate oral enteral intake is impossible.
a. Chronic obstruction of the GI tract uncorrected or not correctable within 10 days in older children, 5 days in children below 5 years old.
- Gastric malignancies pending surgery
- Superior mesenteric artery syndrome
Intestinal atresia
- Malrotation of the bowels
Short bowel syndrome
Post irradiation effects on bowels pending surgery
Chemotherapy complications in bowels pending surgery
Massive catabolism
- Major burns
- Multiple major operations
- Multiple major trauma
•Congenital anomalies compatible with adequate oral intake later in life
- Omphalocoele
- Gastroschisis
- Diaphragmatic hernias
- Abdominal wound dehiscence7
•When oral enteral intake is not advisable
a. High output GI fistulas wherein oral or enteral feeding is inadequate
b. Extremely premature infants with surgical problems
NURSING RESPOSIBILITIES AND CARE OF PATIENT WITH TPN
•Prepare the patient and family emotionally and physically for the procedures.
- Explain procedure to patient and family to allay anxiety in developmentally appropriate terms.
- Allow the child and family to express concerns and feelings.
- Younger children may benefit from therapeutic play with a doll or puppet.
•Assist the physician during the catheter insertion.
- Prepare all materials / equipment needed.
•Ensure that physician’s orders are carried out.
- Check solution content with orders to ensure correct hyperalimentation solution additive before starting the infusion.
- Each TPN bottle must be labelled with patient’s name, room number, additives, IV number, date starting time and time to consume.
•Ensure that patient will receive adequate nutrition
- Monitor the volume/amount of solution hourly
- Inspect the peripheral TPN site for evidence of infiltration


My name is hoover, my 18 years old daughter, Tricia was diagnosed of herpes 3 years ago. ever since then,we have been going from one hospital to the other. We tried all sorts of pills but all efforts to get rid of the virus was futile. The blisters kept on reappearing after some months. My daughter was making use of Acyclovir tablets 200mg. 2 tablets every 6hours and fusitin cream 15grams. and H5 POT. Permanganate with water to be applied 2x a day but all still show no result. So I was on the internet some months back, to sought for any other means of saving my only child. just then, i came across a comment on dr imoloa herbal treatment and decided to give it a try. i contacted the him and he prepared some herbs and sent it to me together with guidelines on how to use the herbs through DHL courier service. my daughter used it as directed dr imoloa and in less than 14days, my daughter regained her health.. You should contact Dr imoloa today directly on his email address for any kind of health challenge; lupus disease, mouth ulcer, mouth cancer, body pain, fever, hepatitis A.B.C., syphilis, diarrhea, HIV/AIDS, Huntington's Disease, back acne, Chronic renal failure, addison disease, Chronic Pain, Crohn's Disease, Cystic Fibrosis, Fibromyalgia, Inflammatory Bowel Disease, fungal nail disease, Lyme Disease, Celia disease, Lymphoma, Major Depression, Malignant Melanoma, Mania, Melorheostosis, Meniere's Disease, Mucopolysaccharidosis , Multiple Sclerosis, Muscular Dystrophy, Rheumatoid Arthritis, Alzheimer's Disease, parkison disease, vaginal cancer, epilepsy, Anxiety Disorders, Autoimmune Disease, Back Pain, Back Sprain, Bipolar Disorder, Brain Tumour, Malignant, Bruxism, Bulimia, Cervical Disk Disease, cardiovascular disease, Neoplasms, chronic respiratory disease, mental and behavioural disorder, Cystic Fibrosis, Hypertension, Diabetes, asthma, Inflammatory autoimmune-mediated arthritis. chronic kidney disease, inflammatory joint disease, impotence, feta alcohol spectrum, Dysthymic Disorder, Eczema, tuberculosis, Chronic Fatigue Syndrome, constipation, inflammatory bowel disease. and many more; contact him on email- drimolaherbalmademedicine@gmail.com./ also on whatssap-+2347081986098.
ReplyDelete